Revenue Cycle Management
Maximize Revenue, Minimize Errors, and Streamline Your Practice

Increase Revenue and Reduce Denials by 30%
Our 15 years of Experience can help maximize your healthcare revenue cycle management potential by delivering effective billing solutions that will accelerate your cash flow.
By partnering with us you can give maximum care to your patients while leaving the tedious tasks for us
Why Partner with Medeo Assist for your Billing Needs?
Getting reimbursements on time depends on accurate medical billing and coding—just one small mistake can hold up payments. Billing and coding are crucial for healthcare providers but handling them can take valuable time away from patient care.
Medeo Assist takes the burden of billing and coding off your shoulders, allowing you to focus on what matters most caring for your patients. Our team of experienced professionals ensures every claim is coded accurately and submitted promptly, minimizing errors and preventing payment delays.
Our Revenue Cycle Features
- HIPPA and PHI Compliant
- Dedicated Account Manager
- Certified Billing and Coding Team
- Real Time Claim Tracking
- 98% Claim Submission Within 24 hours
- Rejection Follow up within 24 hours
- Payment Posting to Maintain Accuracy


Where Do Practices Loose Money?
- Mostly up to collecting the “easy” dollars; ignoring “hard” dollars not reaching the true potential of Practices.
- Out-dated knowledge of robust changes in billing and coding guidelines, government regulations and payer trends.
- Underpayment by healthcare payers is a common problem.
- Lack of accurate and complete patient demographic information results in the practice’s inability to submit a clean claim.
- Average revenue loss of 10%-20% due to insurance claim rejections.
- Practices only collecting less than 50% patient balances owed.
what our clients say
Ready To Transform Your Billing Process?
We’re here to support your practice. Fill out the form below to book a free consultation.
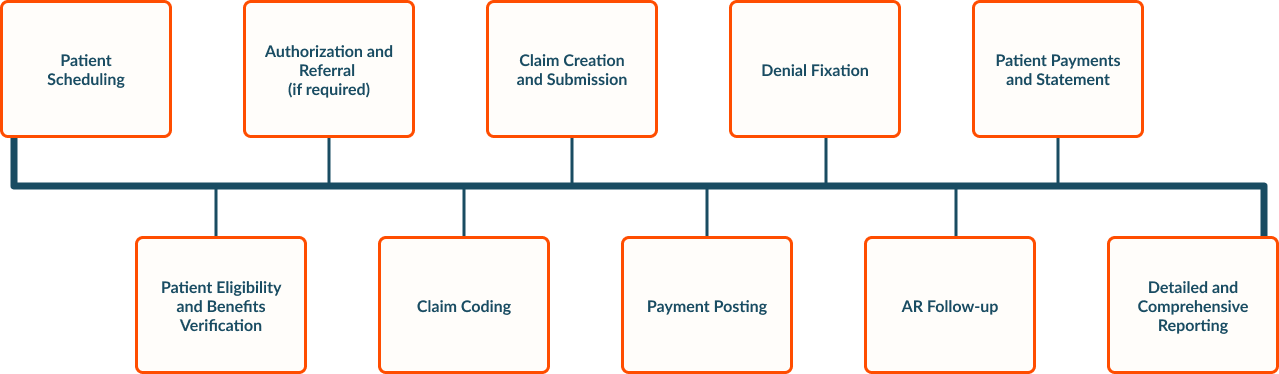
8 Step Success System