Medical Credentialing Services

Effortless Credentialing to Expand Your Practice Reach
Medeo Assist makes credentialing straightforward and stress-free, helping you quickly secure partnerships with payers and expand your reach to more patients. Our team takes on the full credentialing process—from initial paperwork through final enrollment—ensuring everything is accurate, up-to-date, and fully compliant. With our 15 years of expertise, you can skip the back-and-forth with insurers and get your practice credentialed efficiently, giving you more time to focus on patient care and practice growth.
Why Choose Professional Medical Credentialing?
Professional medical credentialing streamlines the complex process of verifying healthcare providers’ qualifications, freeing them from administrative burdens and allowing them to focus on patient care. Credentialing is essential for healthcare organizations, as it ensures providers meet industry standards, licensing requirements, and insurance policies, contributing to high-quality patient care and compliance.
Our Credentialing and Enrollment Services simplify this process by handling every step with precision and expertise. From initial applications to renewals and re validations, we take care of each stage, accelerating the credentialing journey and making it stress-free. With our support, healthcare providers and organizations can confidently navigate credentialing, knowing every detail is managed effectively.
What We Offer in Credentialing

Unlocking the Power of Credentialing & Enrollment Services
Medeo Assist offers comprehensive, end-to-end credentialing and enrollment services, ensuring seamless management of the process with expert industry knowledge. We ensure compliance with payer requirements and provide tailored solutions for both individual and group practices. Our services include real-time updates, clear communication with payers, and a proactive approach to maintaining provider compliance and eligibility. With customized solutions for telemedicine, lab services, and payer fee schedules, Medeo Assist adapts to meet the unique needs of every healthcare provider.
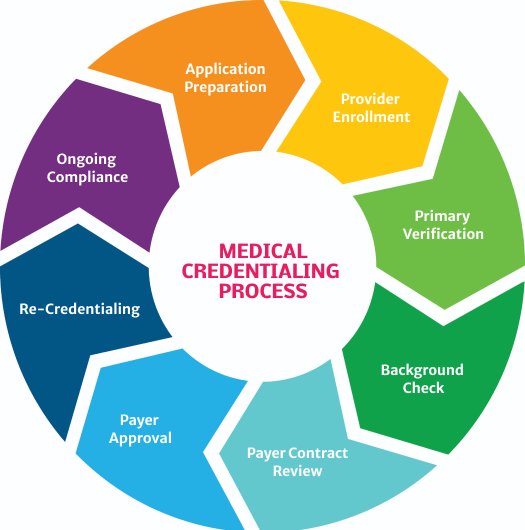
Medical Credentialing Process
Application Preparation
Gather your essential documents—licenses, board certifications, and insurance info—to get started.
Provider Enrollment
We’ll submit applications to insurers and government payers like Medicare and Medicaid on your behalf.
Primary Verification
Credentialing teams verify your licenses, education, and certifications directly with primary sources.
Background Checks
Conduct thorough checks to review any past claims, criminal history, or license sanctions.
Payer Contract Review
Review and negotiate payer contracts to ensure competitive rates and clear terms.
Payer Approval
After review, insurers will approve your enrollment, which may take a few weeks.
Re-Credentialing
Every 1–3 years, you’ll re-credential to stay in-network and compliant with updated requirements.
Ongoing Compliance
We’ll help you keep all your credentials and certifications current, so you’re always in good standing.
Ready To Transform Your Billing Process?
We’re here to support your practice. Fill out the form below to book a free consultation.
